BONE DENSITY SCANS ARE INACCURATE AND BIASED TOWARDS SLIM WOMEN
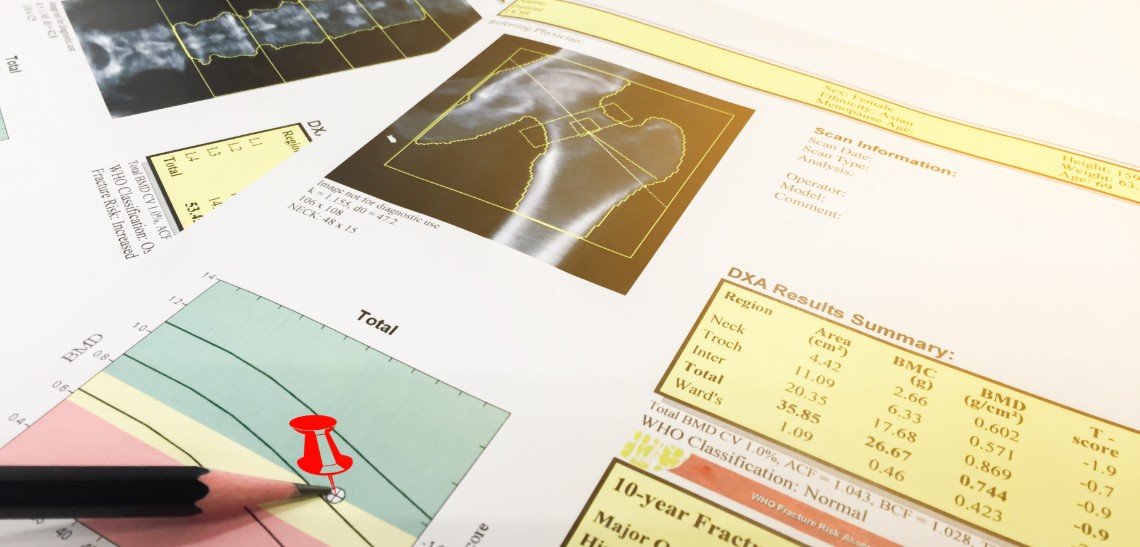
Bone density scans are carried out to determine if a patient is suffering from osteopenia or osteoporosis. Osteopenia is widely regarded to be a precursor to osteoporosis. Both are characterised by lower-than-normal bone density.
If either of these conditions are diagnosed, medication will be prescribed to strengthen the bones with the aim of preventing future fractures. However, there is ample scientific and clinical evidence that the bone density scan is highly unreliable and the recommended therapy for both osteopenia and osteoporosis is not only ineffective but deadly to bone health.
What is wrong with a DEXA scan?
Several studies have shown that DEXA scans do not produce cohesive and accurate reports. The scanners themselves are essentially X-ray machines for the bones.
Shockingly, the technology has not moved on in terms of its design since the 1980s. This puts it completely out of line with all technological progress that has occurred over the last three decades. Perhaps this would not be too bad if the machines were functioning at a high level, but this is not the case.
The seminal problem with DEXA scans is that they produce variable results. Studies have confirmed that DEXA scan reports differ from one machine to another and can change depending on variable factors. For example, the time of day, the immediate physical activity of the patient, the temperature etc.
Effectively this means that something as simple as going for a morning jog before having one of these tests will alter the result.
One of the most worrying aspects of the DEXA scan is that the report is negatively biased against thinner women. Women who have larger frames are given a healthier report by the scan than slimmer women.
Studies show that the DEXA scan makes many wrong diagnoses of osteoporosis and osteopenia in smaller women, leading to unnecessary treatment.
Dangerous medication and how it affects the natural bone cycle
This leads us onto the next big problem: the medications that are prescribed when osteoporosis or osteopenia is detected by the inaccurate DEXA scan.
These drugs belong to a class known as bisphosphonates, which include drugs such as alendronates and ibandronate or ibandronic acid. To understand why they pose a threat to health, it is first necessary to understand the natural life cycle of the bones.
Our bones are not static, they continuously repair and regenerate themselves. This renewal process is done using two sets of cells – osteoclasts that produce new bone cells and osteoblasts that dissolve old bone. An easy way to remember the difference between the two is that osteoblasts ‘blast away’ the old cells.
Drugs that are prescribed for osteopenia and osteoporosis, such as alendronate, inhibit the osteoblast cells. This prevents the dissolution of old bone. The osteoclast cells continue to function as normal, meaning that new bone is formed on top of the old. When a DEXA scan is run, it will report that the bones have thickened and are denser as a result of the medication. While this may sound like a positive development, it is actually very harmful.
When new bone is built on top of old bone that would have been dissolved had the body’s natural regeneration process been allowed to function as normal, the resulting bone structure is actually weaker – even though it appears to be thicker on a DEXA scan. This is because the old bone is not strong. It has the same effect as building a new house on old foundations that are worn and weathered from time.
Is there a safe alternative treatment?
Our bones and joints become weak and diseased when their supporting structure is not as sturdy as they need to be. Using the house metaphor, it does not matter how strong the walls are or how good the roof is if the foundations are not sturdy the house will not stand for long. In the body, the supporting structure is a protein called collagen.
The most important mineral the body requires to produce collagen is MSM (Methyl Sulphonyl Methane). The joints also require other nutrients such as calcium, magnesium, silica, boron, zinc, vitamin C and vitamin D. Whilst you can get all of these nutrients by eating a good diet, MSM has become a problem in recent times because it is missing from our food due to changes in farming processes.
This is why taking MSM is a good idea, however, not all forms are equal. Supplementary tablets are derived from animal protein and are difficult for the body to digest, meaning that it cannot extract the amount that these products claim to provide. The optimal way of taking MSM is in powder form. This also has the benefit of being more cost-effective than in tablet or capsule form.
Taking MSM
An effective dose for treating joint pain and bone aches is two teaspoons of MSM powder in a glass of water taken twice daily for three months. To help the absorption process, you should have a small portion of fruit immediately afterwards. A few segments of orange or a handful of berries, for example. This will also help with the flavour of the powder, which is not overly pleasant. The pain relief it brings is typically noticeable within a couple of hours to a few days. You can also dissolve the powder in fruit juice to improve its taste.
The dose for maintaining and strengthening the bones and joints and preventing against disease is one teaspoon in a glass of water in the morning and afternoon. Again, follow this with a small portion of fruit.